NAP6 FAQs

Please click on the Frequently Asked Questions below to expand each answer.
If your question is not covered in the below FAQs, please contact us.
1. If a patient suffers anaphylaxis in a nearby private hospital theatre and is transferred to a NHS hospital HDU, should this case be included? Also we have an NHS-provided private ward/facility here. Are these cases included?
For the purposes of NAP6, the private ward would be deemed to sit within the NHS hospital and as such is included. However, an entirely separate private unit stationed on or close to the NHS hospital would be excluded.
2. Are local/regional procedures excluded (unless done under sedation or if GA is co-administered)?
The inclusion criteria have been widened and all cases attended by an anaesthetist are now included. Please see the updated LC information pack which is available to download on our website http://www.nationalauditprojects.org.uk/NAP6-Resources).
3. Where will bone cement implantation reactions fit into NAP6, mimicking as they do anaphylactoid reactions?
If the timing of the reaction strongly suggests Bone Cement Implantation Syndrome such that anaphylaxis is not suspected, it is not necessary to report the case to NAP6. However, if anaphylaxis is suspected (or indeed part of a differential diagnosis) the case should be reported.
4. Are cases that have been done under local anaesthetic or regional block with no sedation, for example Caesarean section under spinal anaesthesia, included?
Yes these are now included. Please see updated inclusion criteria below. (This information is contained on page 2 of the LC information pack).
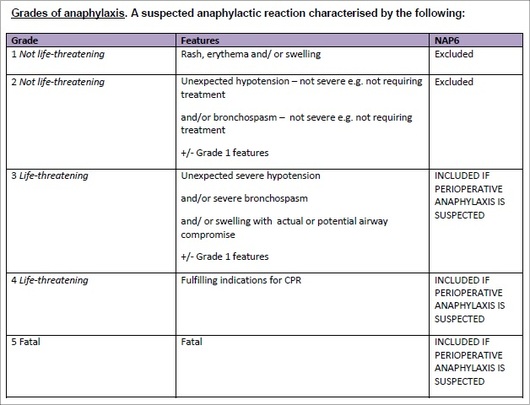
Click image to expand
5. Are children included?
Yes, NAP6 will collect reports of severe (i.e. life-threatening) anaphylaxis in adults and children
6. What is the NAP6 definition of 'Perioperative Anaphylaxis'?
Anaphylaxis which occurs:
- In a patient undergoing a procedure requiring general or regional anaesthesia or sedation or managed anaesthesia care (anaesthetist monitoring only)
and
- Under the care of an anaesthetist
and
- Between the period of first administration of a drug (including pre-med) and the post-procedure transfer to the ward, HDU or ICU
7. Grade 2 anaphylaxis states hypotension/bronchospasm not requiring treatment. If a patient receives simple treatment like any vasopressor (ephedrine/metaraminol/ phenylephrine) or salbutamol nebs for bronchospasm, are they excluded?
The definitions in the table (below) are pragmatic. Remember that all the definitions start with 'suspected anaphylaxis'. If anaphylaxis is not suspected, there is no need to report the case to NAP6. There is an element of judgement in deciding whether hypotension (or bronchospasm) was mild or severe and hence whether the case was Grade 2 or 3. To aid judgement we have described grade 2 as 'e.g. not requiring treatment'. However it may be that someone with relatively mild hypotension and suspected anaphylaxis receives modest doses of a vasopressor or fluid. This might still be consistent with 'mild hypotension'. Hypotension that is profound, sustained, resistant to treatment or requires extensive treatment is 'severe' and thus the case is grade 3.
8. What paperwork is needed for the first snapshot in November?
The Baseline Survey will be carried out in November. This is an on-line survey for all anaesthetists to complete. As LC, you will asked to email a link to all the anaesthetists in your hospital requesting that they complete the survey on-line. It is important that they send you an email confirming that they have completed the survey, so that you know who you need to chase-up. NAP6 is currently only collecting information about perioperative anaphylaxis occurring in NHS hospitals. Patients who experience anaphylaxis in private hospitals are excluded, even if they are transferred to an NHS hospital for HDU/ICU care. Independent sector hospitals are currently being surveyed to consider (deferred) inclusion and we will be sending further information on this in the future.
9. Are immunologists also going to enter data, have they been informed separately already?
Data will not be entered by immunologists and allergists. The reporting form will be in two parts: In part A, the case details will be reported. In part B, the LC/reporting-anaesthetist will enter the information provided by the allergy clinic in their clinic letter after the patient has undergone investigation. Allergists and immunologists will be aware of NAP6 because a survey of allergy clinics will take place, but they will not be asked to enter any information about specific cases.
10. Are HDU, ICU and the Emergency Department included?
Yes, but only if the patient received a general anaesthetic for an interventional procedure (not resuscitation) administered by an anaesthetist.
10b. Many patients go to radiology for a prolonged investigations - are these excluded unless they involve interventional angio or Ct guided biopsy? Does an already-anaesthetised patient on CC (perhaps there for weeks already), who then has a reaction to a drug or i.v. contrast, warrant reporting?
We are interested in patients undergoing interventional procedures under general anaesthesia while critically ill. The definition of interventional procedure in critical care patients is frankly rather arbitrary, as is the boundary between heavy sedation and light anaesthesia.
The following would be interventions:
- Tracheal intubation
- Tracheostomy
- Insertion of chest drain
- Lumbar puncture
- Percutaneous drainage of abscess
- Radiological or cardiac procedures
If the patient was continuously sedated and required the level of sedation to be deepened to the level of anaesthesia - i.e. complete insensibility, then we would class this as general anaesthesia. In our experience it would be very rare for a patient to be anaesthetised for a prolonged period (as opposed to sedated). If the procedure was performed under sedation +/- local anaesthesia, it would not be included. To answer specific examples:
- Transfer to radiology for scan or interventional radiology
- Included if done with GA
- Excluded if sedated
If there is significant doubt, feel free to discuss the case in confidence via email with the NAP6 Moderator
11. In some areas like endoscopy - the surgeons and endoscopist provide sedation to the patients. Any allergic reaction noted or occurring in that setup is not included in our audit - is that right?
Yes, we are only including cases under the care of an anaesthetist at the time of the reaction.
12. Where can I find the audit protocol with details of the methodology, data collection items etc?
13. When will you send out paperwork for the baseline survey?
The Baseline Survey will be carried out at the beginning of November 2015. We will send more detailed directions in the near future. This is an on-line survey for all anaesthetists to complete; there is no paperwork for this part of NAP6. As LC, you will asked to email a link to all the anaesthetists in your hospital requesting that they complete the survey on-line. It is important that they send you an email confirming that they have completed the survey, so that you know who you need to chase-up.
14. Are there any recommendations as to how much SPA time should be allocated to NAP projects?
It is our view that all activity related to the NAP6 Local Coordinator role is valid for inclusion in SPA activity, and should be used to help support the SPA allocation in consultant and career grade job plans (noting that 2.5 SPAs are regarded as 'typical' in the 2003 Consultant Contract Terms and Conditions). Where doctors who wish to act as Local Coordinators are prevented from doing so by inappropriate allocation of SPAs, or where Trust/ Boards fail to recognise this activity as appropriate for SPAs, the College will provide evidence in support of relevant activity. In recognition of the role played by the NAP Local Coordinators we will send you a certificate confirming the role, which you may include in your personal portfolio.
15. What time commitment is required from LCs?
As the arrangements between hospitals vary it is difficult to ascertain a set amount of time required. However, it may be useful to get in touch with the previous LC from NAP5 to find out their experience of reporting in the last NAP within your hospital or Trust. As the duties will be very similar to NAP5, a feedback survey from NAP5 confirmed that LCs took on average an hour per week to perform the required data collection. Please refer to the LC information pack for key information containing the timelines.
16. When is NAP6 expected to start and finish?
The NAP6 data collection window starts on 5th November 2015 and runs for one year until 5th November 2016. LCs will have until March 2017 to submit details of cases occurring within this window.
Please see the project outlines in LC guide and Powerpoint presentation for further details.
17. Will NAP6 occur in Republic of Ireland as NAP5 did?
Ireland is not taking part in NAP6.
18. Does the baseline survey include only anaesthetic trainees? What about ACCS /Foundation Year 2 trainees who cover ICU and occasionally come to theatres?
The Baseline Survey will collect information from anaesthetists, including trainees about their experience of perioperative anaphylaxis during the previous 12 months, as well as local management and referral pathways and individual perceptions. We ask respondents to include only cases where they were the most senior anaesthetist present, to avoid double-reporting. In practice, this means that individuals who only give anaesthetics under supervision will not be able to complete the Survey.
19. How can anaesthetists retired from the NHS but working privately be involved?
Thank you for your interest in contributing to NAP6. Please see the Independent Hospitals page for more information on private sector hospital involvement with NAP6.
20. Should the NAP6 Local Coordinator should be responsible for referring patients for further investigation and corresponding with the patient, surgeon and GP?
No. An important tenet of NAPs is that they do not change current practice during the data collection period. The anaesthetist present at the time of the anaphylactic reaction is normally responsible for management and subsequent follow-up. This includes referring the patient for investigation, all correspondence, and obtaining the results of all relevant investigations.
21. Should the departmental Clinical Lead for perioperative anaphylaxis relinquish this role if they are also the Local Coordinator for NAP6?
Current local practice should not be changed. Many anaesthetic departments have a Clinical Lead for perioperative anaphylaxis. If the departmental Clinical Lead becomes the Local Coordinator for NAP6, they can fulfill both roles.
22. Are PA(A)s expected to fill in a form in the Activity/Allergen survey phase?
Baseline Survey:
As PA(A)s are not anaesthetists providing independent care of patients, they should not be included in the Baseline survey.
Reporting of cases of suspected anaphylaxis (main data collection):
Where PA(A)s are supervised in accordance with the RCoA guidance on PA(A)s, the patient's care will remain under the direct supervision of a consultant anaesthetist. Therefore anaphylaxis occurring during these cases should be reported to NAP6. Where supervision falls outside this guidance - i.e. distant supervision - the case does not meet inclusion criteria for NAP6 as the patient is not under the direct care of an anaesthetist.
Activity/Allergen Survey:
As for main data collection (see above).
Yes, this cases should be reported to NAP6 - they fall within the guidance.
Last updated 29th October 2015.